Can frailty, locomotive syndrome, and sarcopenia be treated?
Frailty, locomotive syndrome, and sarcopenia are interconnected conditions. Frailty is characterized as a state of increased vulnerability resulting from age-related decline in reserve and function across multiple physiological systems, leading to a compromised ability to cope with stressors. Locomotive syndrome is characterized by reduced mobility resulting from dysfunction in locomotive organs, such as osteoporosis, which heightens fracture risk, and sarcopenia, a condition marked by skeletal muscle wasting. The prevalence of these conditions rises with age and is associated with a higher risk of morbidity and mortality. Current evidence suggests that exercise, rehabilitation, and nutritional interventions are the most effective strategies for managing these conditions and their key components. In some cases, pharmacological interventions can prevent, delay, reverse, or reduce the severity of these conditions. Comprehensive geriatric interdisciplinary assessments and treatments, including addressing lifestyle-related diseases, have been shown to improve health outcomes in frailty and its components. Medical treatments for osteoporosis, a major component of locomotive syndrome, have been proven to reduce fracture risk and enhance patients’ quality of life.
Relationship between lifestyle-related diseases and frailty, locomotive syndrome, sarcopenia
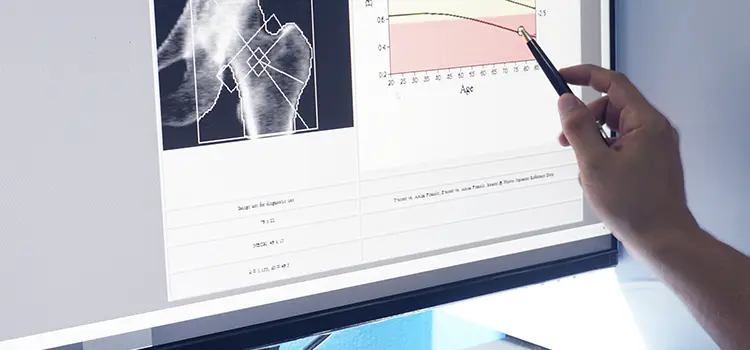
Osteoporosis, sarcopenia, and cognitive impairment, which are components of frailty and locomotive syndrome, are closely linked to lifestyle-related diseases such as diabetes, atherosclerotic disease, and chronic kidney disease. Current data reveal a complex relationship between lifestyle-related diseases and frailty, locomotive syndrome, and sarcopenia, underscoring a bidirectional and mutual association between these entities (Fig. 1).

For instance, unstable blood glucose levels, particularly hypoglycemia, have been shown to be major risk factors for sarcopenia, cognitive decline, falls, and fractures in patients with diabetes. In contrast, some anti-diabetic medications increase the risk of falls and fractures, necessitating caution in patients with a high risk of sarcopenia. Medication adherence may be lower in patients with cognitive impairment, leading to poor clinical and economic outcomes. Furthermore, osteoporotic fractures and cognitive decline can result in decreased physical function and muscle mass, contributing to poor diabetes control and an increased risk of additional fractures. Given the prevalence of comorbid conditions in elderly patients, as shown in Figure 1, comprehensive diagnosis and treatment by physicians are essential. Our department offers a highly specialized approach to lifestyle-related diseases, including diabetes, atherosclerotic disease, chronic kidney disease, and osteoporosis, with a focus on interventional treatments to prevent the progression of frailty, locomotive syndrome, and sarcopenia.